Key Healthcare AI Trends Shaping Innovation in 2026
Top Healthcare AI trends for 2026: predictive care, automation, diagnostics, and innovation.


Healthcare in 2026 is no longer defined by incremental upgrades—it’s being rebuilt around intelligent systems, predictive engines, and autonomous tools that reshape how care is delivered, financed, and experienced. As global medical spending climbs and labor shortages intensify, leaders are turning to AI in healthcare not as an optional efficiency add-on, but as a core strategic pillar for sustainability, quality, and patient access.
Across hospitals, payers, and life sciences, AI Innovation is maturing from pilot projects to enterprise-wide transformation. Intelligent automation is lowering administrative waste, multimodal models are elevating diagnostics, and connected data platforms are powering proactive care. Innovations that once sounded experimental—virtual hospitals, synthetic health data, CRISPR-AI copilots—are now quietly entering mainstream operations.
Below is a data-driven, expert breakdown of the Healthcare AI trends that will define 2026 and beyond.
Health System Execs Are Prioritizing AI. Read more here!
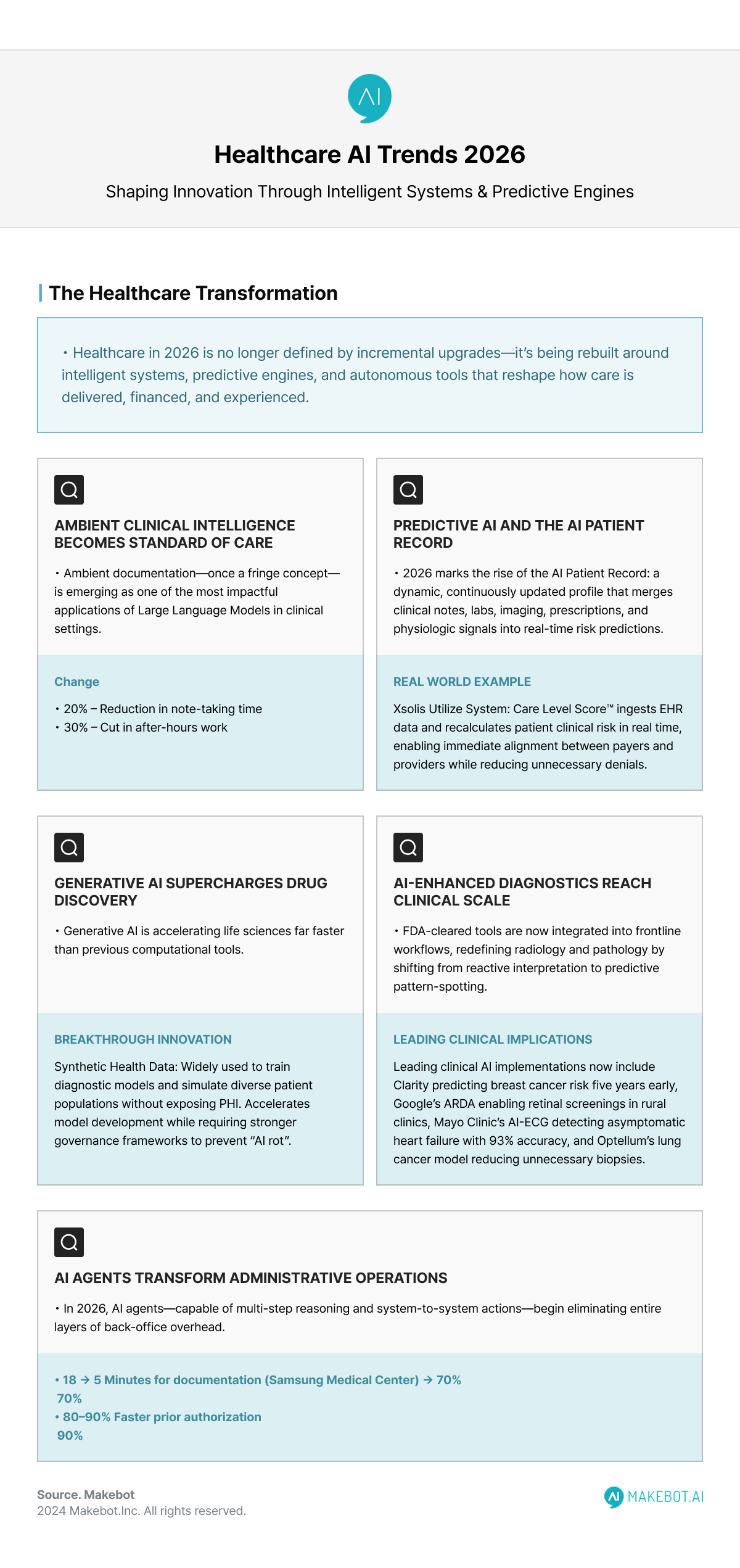
1. Ambient Clinical Intelligence Becomes a Standard of Care
Ambient documentation—once a fringe concept—is emerging as one of the most impactful applications of Large language models in clinical settings. Advanced ACI systems automatically capture, structure, and summarize patient-clinician conversations, removing one of the biggest drivers of clinician burnout: medical documentation.
Studies show AI-augmented documentation reduces note-taking time by up to 20% and cuts after-hours work by 30%. Systems such as Nuance DAX Copilot and Xsolis-powered tools now integrate directly inside EHR workflows, achieving real-time accuracy that previously required multiple staff touchpoints. Early adopters report significantly lower error rates and more consistent utilization reviews.
As staffing shortages intensify through 2026, ACI will shift from “nice to have” to a clinical necessity—especially for primary care and behavioral health teams stretched beyond capacity.
2. Predictive AI and the Emergence of the AI Patient Record
2026 marks the rise of the AI Patient Record: a dynamic, continuously updated profile that merges clinical notes, labs, imaging, prescriptions, and physiologic signals into real-time risk predictions.
Platforms like Xsolis’ Utilize system already demonstrate this transformation. Its Care Level Score™ ingests EHR data and recalculates a patient’s clinical risk in real time, enabling immediate alignment between payers and providers while reducing unnecessary denials.
This shift fundamentally changes utilization management:
- Faster detection of deterioration
- Unified decision-making between clinicians and insurers
- Reduced friction across the payer-provider ecosystem
- Proactive intervention over retrospective chart review
In 2026, predictive analytics powered by LLM-based context engineering will become a default requirement in modern EHR platforms.
3. Generative AI Supercharges Drug Discovery and Synthetic Health Data
Generative AI is accelerating life sciences far faster than previous computational tools. After breakthrough successes in 2025, researchers will deploy multimodal AI to:
- Screen billions of molecular candidates
- Simulate drug-target interactions
- Predict toxicity and metabolic pathways
- Optimize trial designs
This shift enables pharmaceutical companies to reach clinical trial readiness with unprecedented speed. Synthetic health data—another branch of Generative AI—is now widely used to train diagnostic models and simulate diverse patient populations without exposing PHI.
The industry is seeing both reward and risk: while synthetic data accelerates model development, the threat of “AI rot” (models trained on synthetic-only loops) requires stronger governance frameworks in 2026.
4. AI-Enhanced Diagnostics Reach Clinical Scale
AI-assisted diagnostics are moving beyond pilots into widespread clinical deployment. FDA-cleared tools for breast cancer risk prediction, retinal disease detection, and cardiac dysfunction are now integrated into frontline workflows.
Examples include:
- Clairity predicting breast cancer risk five years in advance
- Google’s ARDA enabling retinal screenings in rural clinics
- Mayo Clinic’s AI-enhanced ECG detecting asymptomatic heart failure with 93% accuracy
- Optellum’s lung cancer model reducing unnecessary biopsies
These solutions redefine radiology and pathology by shifting from reactive interpretation to predictive pattern-spotting. In 2026, AI-diagnostic copilots will support clinicians in nearly every major imaging modality.
5. AI Agents Transform Operations, Scheduling, and Administrative Workflows
Administrative inefficiency remains a quarter-trillion-dollar annual burden in U.S. healthcare. In 2026, AI agents—capable of multi-step reasoning and system-to-system actions—begin eliminating entire layers of back-office overhead.
Key impact areas include:
- Prior authorization automation (80–90% faster approval times)
- Claims processing, discrepancy detection, and automatic coding
- Self-scheduling systems leveraging predictive demand
- Intelligent routing of clinical tasks
Hospitals like Samsung Medical Center cut documentation issuance times from 18 minutes to 5 by deploying robotic process automation. Payers and providers are also aligning through shared AI-generated insights, improving transparency and reducing denial rates.
In an industry plagued by workforce shortages, agentic AI becomes a force multiplier.
The Future of AI in Healthcare: Insights from Former CDC Director Dr. Rochelle Walensky. More here!
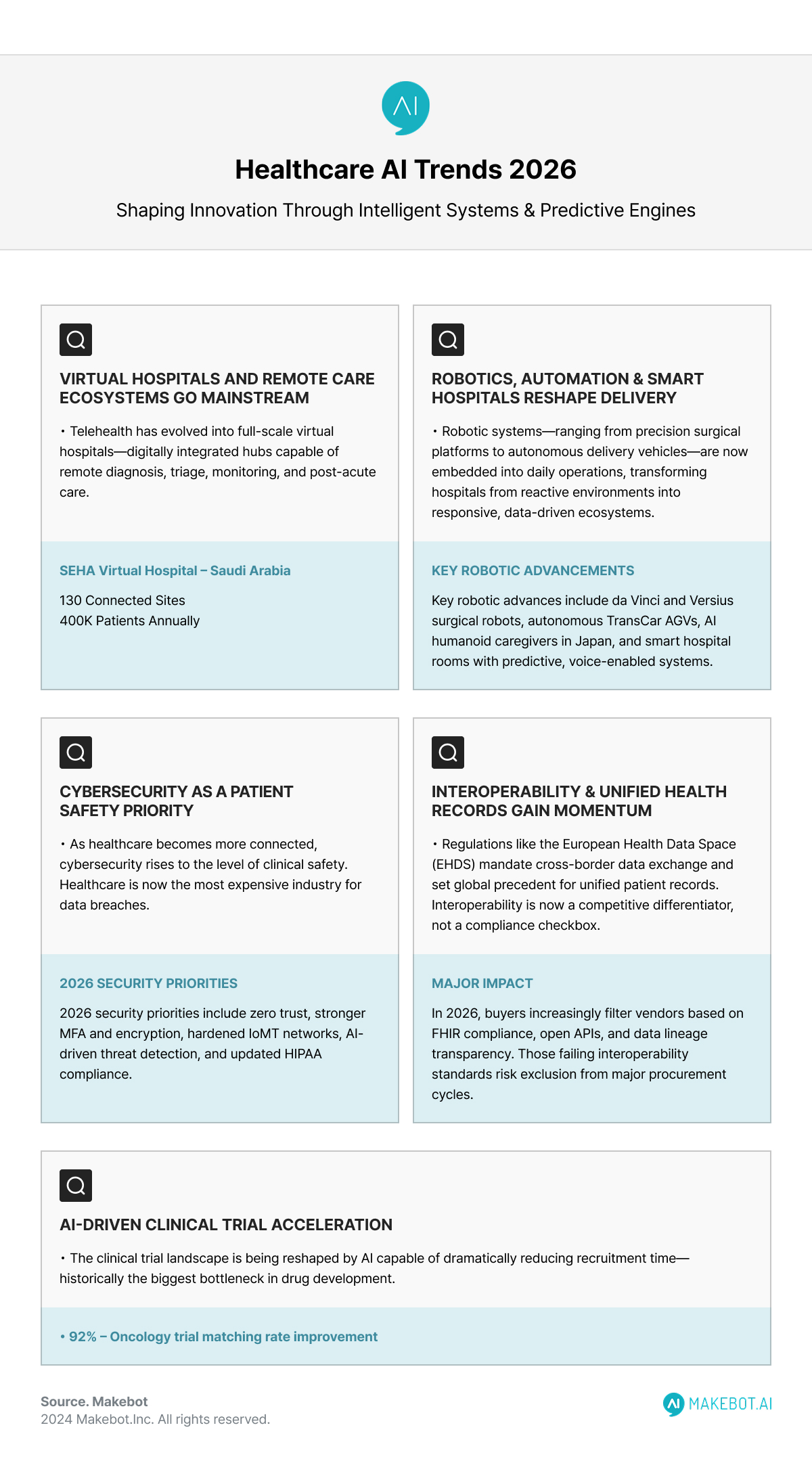
6. Virtual Hospitals and Remote Care Ecosystems Become Mainstream
Telehealth has evolved into full-scale virtual hospitals—digitally integrated hubs capable of remote diagnosis, triage, monitoring, and post-acute care. Saudi Arabia’s SEHA Virtual Hospital now serves 130 sites and treats 400,000 patients annually.
2026 accelerators include:
- AI-driven monitoring from wearables and IoMT sensors
- Continuous data ingestion from home-based devices
- Virtual nursing support for admissions, education, and discharge
- Tele-ICU teams delivering oversight across multiple sites
With an aging population and severe clinician shortages, virtual care becomes a structural solution—not just an alternative care channel.
7. Robotics, Automation, and Smart Hospitals Reshape Care Delivery
Robotic systems—ranging from precision surgical platforms to autonomous delivery vehicles—are now embedded into daily operations.
Key advancements:
- da Vinci and Versius leading minimally invasive surgical robotics
- Autonomous AGVs like TransCar managing 24/7 logistics
- AI humanoid caregivers assisting aging populations in Japan
- Smart hospital rooms with predictive care systems and voice-based controls
Smart hospitals use IoT-integrated infrastructure and predictive AI to anticipate sepsis, standardize imaging quality, monitor bed capacity, and optimize supply chains. These systems transform hospitals from reactive environments into responsive, data-driven ecosystems.
8. Strengthened Cybersecurity as a Patient Safety Priority
As healthcare becomes more connected, cybersecurity rises to the level of clinical safety. In 2024, breaches exposed 275 million health records—81% due to hacking—making healthcare the most expensive industry for data breaches at an average of $10.1M per incident.
2026 priorities include:
- Zero-trust architectures
- MFA and encrypted data exchange
- Hardening IoMT and partner networks
- AI-assisted threat detection and rapid incident containment
- Compliance with new HIPAA Security Rule updates
Cybersecurity investments are no longer IT expenditures—they are core to protecting clinical continuity, patient trust, and regulatory posture.
9. Interoperability and Unified Health Records Reach Regulatory Momentum
Regulations like the European Health Data Space (EHDS) mandate cross-border data exchange and set global precedent for unified patient records. Interoperability is now a competitive differentiator, not a compliance checkbox.
Interoperable ecosystems enable:
- Personalized and genomic medicine at scale
- Research acceleration through shared real-world evidence
- Seamless patient transitions across providers
- Reduced errors and redundant tests
In 2026, buyers increasingly filter vendors based on FHIR compliance, open APIs, and data lineage transparency. Those failing interoperability standards risk exclusion from major procurement cycles.
10. AI-Driven Clinical Trial Acceleration
The clinical trial landscape is being reshaped by AI capable of:
- Rapid patient-trial matching
- Protocol optimization via simulations
- Predicting dropout risks or adverse reactions
- Increasing diversity in participant populations
Tools such as TrialMatchAI and Opyl’s TrialKey improve oncology trial matching rates up to 92%, dramatically reducing recruitment time—historically the biggest bottleneck in drug development.
In 2026, AI-optimized, data-driven trial design became standard practice for biopharma.
Implications for Healthcare Leaders in 2026
Operational leaders
Must prioritize AI agents and automation to stabilize workforce challenges.
Clinical leaders
Should integrate ACI and AI-diagnostic copilots directly into EHR workflows, not as standalone tools.
Payers and managed care organizations
Can use predictive analytics to enable aligned decision-making, reduce denials, and enhance value-based contracting.
Life sciences executives
Will increasingly rely on Generative AI for molecular discovery, trial optimization, and synthetic data generation.
CIOs and CTOs
Need to embed cybersecurity, interoperability, and cloud-native AI capabilities as core architectural requirements—not future upgrades.
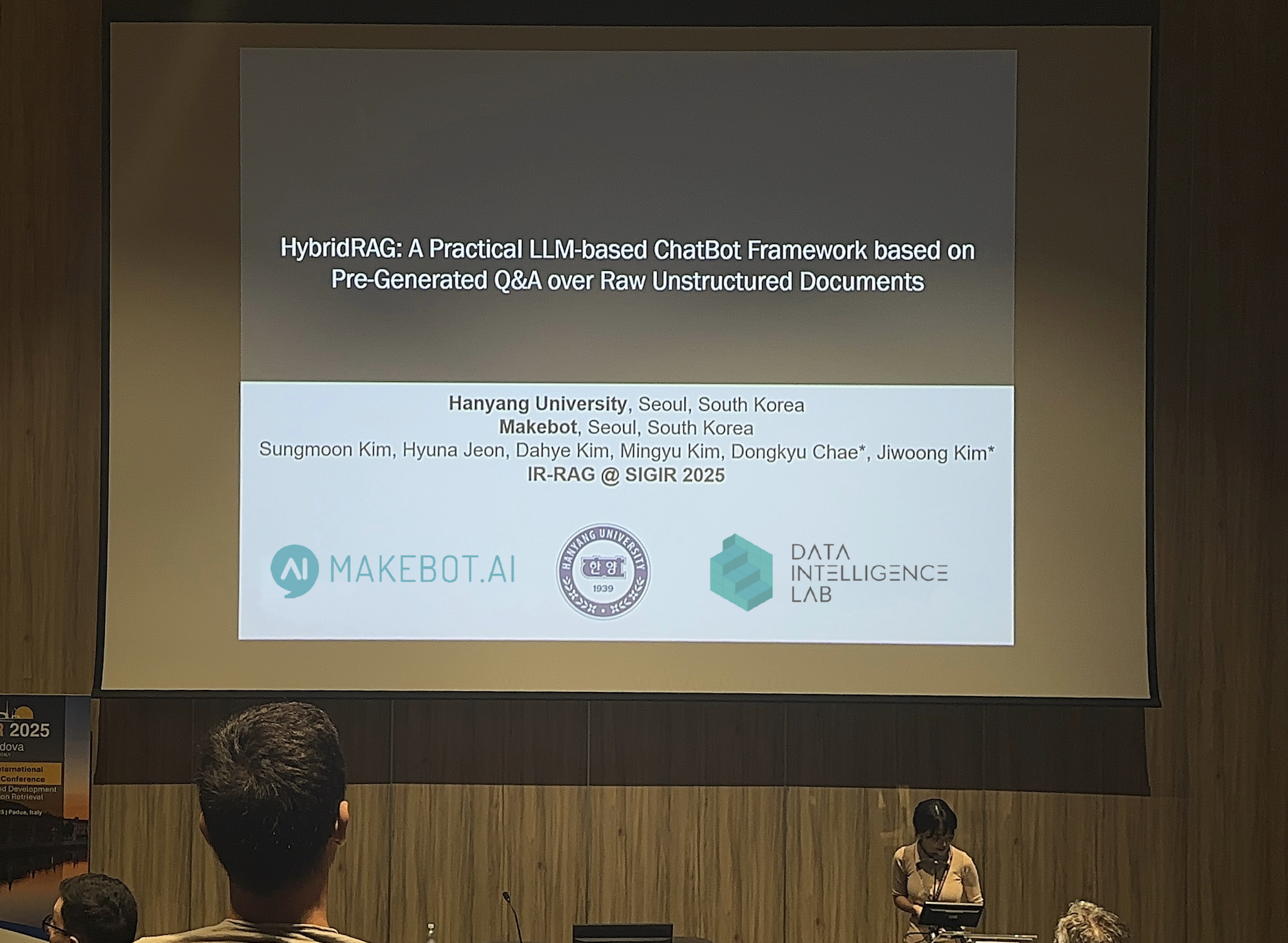
Showcasing Korea’s AI Innovation: Makebot’s HybridRAG Framework Presented at SIGIR 2025 in Italy. More here!
Future Outlook
By 2026, the most competitive healthcare organizations will not simply “use AI”—they will be AI-native. Care will shift from episodic to continuous, from reactive to predictive, and from burdened to augmented.
Large language models, multimodal AI, robotics, edge intelligence, and virtual hospitals will collectively define this new healthcare infrastructure. And as the industry converges around unified data standards, global interoperability, and secure ecosystems, healthcare will move closer to delivering the long-promised ideal: high-quality, personalized, accessible care—at scale.
The transformation is already here. The winners will be those who execute early, invest strategically, and build AI literacy across their workforce.
Makebot: Powering the Next Wave of Healthcare AI
Healthcare’s shift toward predictive, automated, AI-native systems demands more than generic tools—it requires domain-trained intelligence that understands clinical workflows, compliance requirements, and real-world operational constraints. This is where Makebot bridges the gap. We deliver industry-specific LLM agents, multimodal automation, and enterprise-grade AI infrastructure designed for hospitals, insurers, and life sciences organizations moving toward 2026’s new standard of intelligent care.
With HybridRAG, globally validated at SIGIR 2025, Makebot delivers a proven 26.6% accuracy boost and up to 90% cost reduction, empowering health systems to scale Generative AI safely and efficiently. Whether you’re enhancing patient communication, automating documentation, deploying clinical copilots, or integrating predictive analytics, Makebot provides the end-to-end solutions trusted by Seoul National University Hospital, Gangnam Severance, and over 1,000 enterprises worldwide.
👉 Start your AI healthcare transformation today: www.makebot.ai
📩 Contact us: b2b@makebot.ai

Studies Reveal Generative AI Enhances Physician-Patient Communication














































_2.png)


















.jpg)




























